Implant research

Foto: Mikael Wallerstedt
Thanks to excellent results, the insertion of joint prostheses has become a success story and in Sweden, the number of hip prostheses being inserted almost matches the number of balloon angioplasty being performed.
The most common reasons for hip replacements are two common problems, joint diseases and fractures to the femoral neck. Knee replacements are often conducted following joint diseases.
Yet despite 17,000 primary hip replacements and 16,000 knee replacements being conducted each year, the number of patients experiencing serious complications is also increasing. In the two years following a joint prosthesis, infection is a very common reason for repeat surgery, followed by patients with hip replacements that have come out of the hip joint (luxation) being the next most common cause. At later stages, the mechanical loss of prosthetic components is the most common reason for repeat surgery. This often occurs alongside large loss of bone, osteolysis.
The risk of being affected by prosthetic or dislocation following hip replacements has increased in Sweden and in the Nordic region over the last two decades, and it is estimated that each year, at least 500 patients are affected in Sweden. Both prosthetic infections and luxation cause extreme suffering as well as the need for repeat surgery, and mortality rates following prosthetic infection are as high as those of certain cancers. The social costs incurred following prosthetic infections and luxations are high. In addition to the costs to healthcare, the nationwide Swedish insurance company, Löf, make triple-figure payments to the patients affected by these complications.
Much of our prostheses related research addresses preventing, discovering and treating such complications – prosthetic infection, luxation (of hip replacements) and loosening.
The group includes: Hans Malmin, Jan Milbrink, Stergios Lazarinis, Anders Brüggemann, Hannah Eriksson, Andreas Nyström, Demis Kiritopoulos and Yosef Tyson.
Analys av implantatöverlevnad efter höftproteskirurgi.
Some significant projects
1. To identify high-risk patients for prosthetic infection or luxation
The risk of developing prosthetic infection or dislocation is affected by patient-related risk factors: For example, fracture of the femoral neck, diabetes and obesity significantly increase the risk of prosthetic infection. We use large registry data bases to develop support for decisions that can be used in everyday clinical practice to identify high-risk patients. The goal is to develop a simple mobile app that collects information about the patient, and then determine if the patient is at a higher risk of the mentioned complications.
Consequently, these patients may receive individualised treatment through preoperative optimisation of risk factors that may be affected, or undergo surgery under specific safety conditions (individualised antibiotic prophylaxis, implant insertion to reduce the risk of infection or luxation, etc).
2. Developing implants that reduce the risk of prosthetic infection
Each prosthetic infection develops as bacteria adhere to the implant, multiply and encapsulate in a greasy mass known as biofilm, thus making them inaccessible to antibiotics. Cemented implants are protected to a certain extent through the use of antibiotics mixed in with the cement. However non-cemented implants – which are becoming more common – are unprotected. We are working to modify titanium surfaces using nanometre sized silver “islands” and develop resorbable hydrogels containing antibiotics that can be brushed directly onto titanium surfaces. Both strategies will prevent the growth of bacteria and formation of biofilms on non-cemented implants. The strategy can be used both preventatively and as a treatment method for existing infections.
3. Improving the detection of prosthetic infections
Implant-related infection is a devastating consequence of orthopaedic surgery that causes great suffering for the patient and large costs for the healthcare system. Between 1-5 and 5 % of patients are affected by a prosthetic infection following hip or knee arthroplasty depending on whether a person belongs to a risk group such as patients with hip fractures. Diagnostics for determining a prosthetic infection are a challenge. There are several algorithms that support the diagnostic procedure, but no one is completely satisfactory. In about 10-20 % of prosthetic infections, no causative agent can be detected. The identification of causative agents is the key to the successful treatment of orthopaedic infections, hence the relatively high degree of undetectable agents poses a problem.
A significant number of orthopaedic infections are caused by bacteria forming on the biofilm. The biofilm makes using traditional methods to identify bacteria particularly difficult (cultures, including 16S PCR techniques). We are working to investigate and compare if the effect of Dithiothreitol (DTT) or treatment with ultrasound (=sonication) of orthopaedic implants taken out due to suspected infection increases the accuracy of the diagnostics. Treating the removed implants using DTT or sonication releases the bacteria from the biofilm and increases the likelihood that the agents can be identified by cultivation in the lab. Implants that have been removed from patients undergoing revision surgery are treated using sonication or DTT, which is then followed by analyses with conventional cultivation and 16S PCR. The effectiveness of the methods for identifying causative agents is evaluated and compared.
4. Evaluating implants alleged to reduce the risk of luxation
To reduce the risk of luxation, so-called "double cups" have been developed, special joint sockets where a metal shell encloses a larger plastic ball, which in turn grips around the joint prosthesis of the proximal extremity of the humerus. Evaluation of this relatively un-trialled method in Sweden is essential by conducting an expansive, forward-looking study in which at-risk patients are allocated either a regular joint socket or the “double cup”. However, this will require almost 400 patients to be able to explore the technique with sufficient statistical strength, meaning that no single centre can conduct such a study alone.
We therefore intend to perform the first register-based randomised study in Swedish orthopaedics, where high-risk patients throughout Sweden can be randomly assigned to one of the two treatments, i.e. double cups or standard sockets. The allocation, registration and monitoring will take place using the well-established hip arthroplasty register. The most important final outcome is to assess whether the risk of luxation is lower amongst patients allocated a “double cup”.
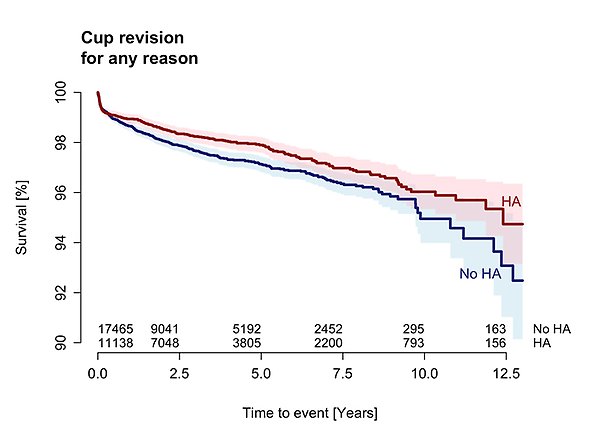
5. Evaluating ways to perform repeat hip joint surgery
We use major register studies to continually work with quality assurance. These studies identify all the patients who underwent repeat surgery of their hip joint or stem, regardless of the cause. Comparisons can then be made between the different implants that were inserted in the repeat surgery in relation to patient and prosthetic survival, post-surgery complications and patient satisfaction. And so conclusions can be reached regarding which patients could benefit from the various implants available. At the same time, we can use this method to identify patient risk factors and therefore provide a more balanced perspective on what any repeat surgery would involve for the individual.
We also evaluate whether patients who undergo surgery with different implants react to the metal used, by analysing the body's immunological response.
