Our research
Our research is mainly focused on molecular imaging and radiation therapy of prostate cancer.
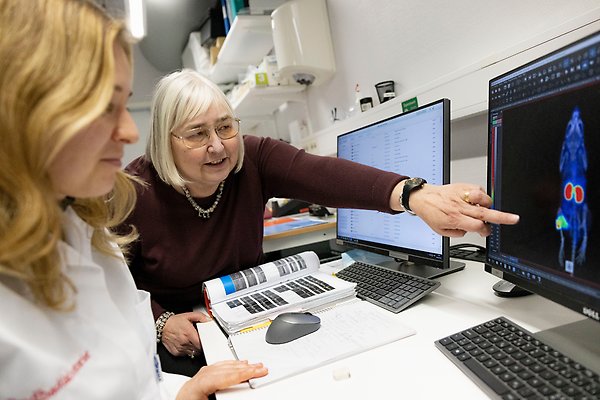
Molecular imaging may improve treatment of prostate cancer by better staging, personalising management and evaluation of therapy response. Our approach to visualization of prostate cancer is radionuclide targeting of the prostate tumour markers.
Correct staging of prostate cancer is crucial for patient management. Conventional anatomical imaging modalities (CT and MRI) tend to understage prostate cancer due to poor sensitivity to soft tissue metastases. The false-negative results contribute to a significant number of patients with extraprostatic disease undergoing non-curative surgery. The use of [18F]FDG for imaging of malignant tumours by positron emission tomography (PET or PET/CT) provides excellent sensitivity in many cancers. However, the utility of this method for prostate cancer is limited because glucose utilisation is low and FDG uptake is insufficient in up to 81% of primary prostate cancers. Other metabolic PET tracers have shown some promising results in the clinic but have low selectivity.
An alternative approach to visualisation of prostate cancer is radionuclide targeting of the prostate tumour marker PSMA. Expression of PSMA is low in normal prostate tissue, but is increased in prostate cancer and correlates with prostate cancer progression. Targeting of PSMA is utilised for imaging of prostate cancer using 111In-labelled ProstaScint (capromab pendetide), which is approved for clinical use by FDA. Still, imaging of PSMA can be improved by both optimizing radionuclide for labelling and by optimizing a tracer format (e.g. the use of small targeting proteins instead of bulky IgG).
Alternative treatments for of androgen-independent prostate cancer could be targeting against tyrosine kinase receptors family that are often overexpressed in advanced prostate cancers. This approach requires confirmation of the presence of receptors in cancer lesions and therapy monitoring for early response. This could be done by radionuclide diagnostic imaging.
Affibody conjugates as alternative to antibodies for tumour targeting
The use of antibodies for diagnostics and therapy has a serious limitation. Antibodies are relatively bulky (170 kDa), which complicates their extravasation and penetration into malignant tissue. Blood clearance is also slow, which causes high background during imaging and high unspecific whole-body irradiation during therapy. Smaller antibody fragments provide better tumour-to-normal tissues radioactivity ratio than intact antibodies and size reduction is a proved approach to improvement of targeting properties of radionuclide probes for tumour imaging and treatment. The size of the immunoglobulin based tracers can only be reduced to 25 kDa for scFv or 15 kDa for domain antibodies.
Affibody molecules are only half the size of the domain antibodies. Affibody molecules are three helical domain proteins of approximately 58 amino acids having a structure deriving from one domain of staphylococcal protein A. Our group participated in selection, evaluation and pre-clinical characterisation of Affibody molecules binding to different molecular targets relevant to prostate cancer, e.g. HER2, EGFR, IGF1R. Preclinical data suggest that the affibody ligand provides at least one order of magnitude better imaging contrast (tumour-to-organ ratios) in murine xenograft model, than the best antibody fragments. The comparison of imaging properties of anti-HER2 ligands as full length antibody trastuzumab and Affibody molecule ABY-025 demonstrated that high contrast image with Affibody molecule can be obtained in much shorter time after injection of radiolabeled ligand probe. Furthermore, clinical data show that 111In- and 68Ga-labelled anti-HER2 Affibody molecule may be used for imaging of HER2-expressing metastases cancer patients.
Theranostics
Anna Orlova, Professor
Theranostics
anna.orlova@ilk.uu.se, +46 (0)73-992 2846
