Nils Welsh
Signaling events that participate in β-cell death, function and regeneration
Both in Type 1 and Type 2 diabetes there is a deficit in the number and function of β-cells. The reasons for increased death and decreased regeneration and function of β-cells remain unknown. Therefore, our overall aim is to study signaling events that participate in β-cell death, function and regeneration. We currently focus on signaling via the non-receptor tyrosine kinase c-Abl, ROS production occurring via the NADPH-dependent oxidases (NOX) and the transcription factor ZBED6, which appears to control β-cell proliferation and function. For these purposes we are studying human β-cells (EndoC-betaH1 cells and human islets) and we utilize techniques such as RNA-seq, CHiP-seq, qPCR, immunoblot analysis, flow cytometry, viral vector-mediated transduction, siRNA and in vivo models.
Role of tyrosine kinases in ß-cell apoptosis and diabetes
It has recently been observed that patients suffering from both leukemia and diabetes were cured from not only leukemia, but also diabetes, when treated with the tyrosine kinase inhibitor Imatinib. (Veneri et al., N Engl J Med. 2005 352(10):1049-50). An anti-diabetic action of Imatinib in Type 2 diabetes is further supported by our recent observation that Imatinib counteracts high-fat diet induced insulin resistance and hyperglycemia in rats (Hägerkvist et al., Clinical Science, (Lond). 2008 114(1):65-71). Moreover, in a study from 2009, Imatinib was also observed to induce remission of diabetes in db/db mice, possibly via decreasing insulin resistance and increasing the ß-cell mass (Han et al., Diabetes. 2009 58(2):329-3). Thus, in both animal models and in Type 2 diabetes patients Imatinib seems to improve glycemic control, possibly via an insulin sensitizing effect.
Imatinib appears to prevent and reverse not only Type 2 diabetes, but also diabetes of animal models with a Type 1 diabetes resembling disease. We have shown that Imatinib protects against ß-cell death in vitro and prevents diabetes in NOD mice and in streptozotocin-diabetic mice, both models for human ß-cell destruction and Type 1 diabetes (Hagerkvist et al., FASEB J. 2007 Feb;21(2):618-28, Hagerkvist et al., Cell Biol Int. 2006 30(12):1013-7). More recently, it has been observed by others that both Imatinib and Sunitinib not only prevented, but also reversed new-onset diabetes in NOD mice (Louvet et al., Proc Natl Acad Sci U S A. 2008 105(48):18895-900). Thus, there exists proof-of-principle in animal models for an anti-diabetic effect of Imatinib and similar tyrosine kinase inhibitors, and that a limited treatment period will not only reverse diabetes, but also mediate long-term protection against re-precipitation of the disease. This has led us (Mokhtari and Welsh, Clin Sci (Lond). 2009 118(4):241-7) and other investigators to propose clinical trials in which Imatinib is given to new-onset Type 1 diabetes patients.
The work by others and us indicates that Imatinib counteracts diabetes via different molecular mechanisms (Figure 1).
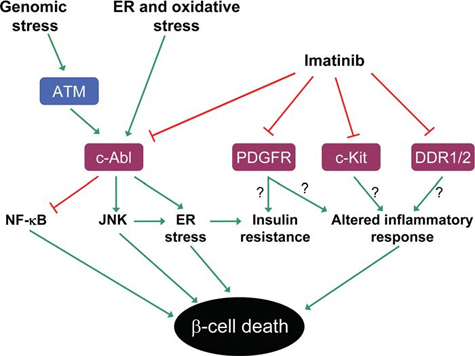
Figure 1 Possible mechanisms for the anti-diabetic effects of imatinib. Imatinib is known to inhibit the tyrosine kinases c-Abl, PDGFR, c-Kit and DDR1/2. Most likely, imatinib-induced protection against diabetes is mediated not by one single pathway, but via different molecular mechanisms. ß-Cell survival is promoted by inhibition of c-Abl, which leads to decreased activation of the pro-apoptotic MAPK JNK and increased activation of the anti-apoptotic transcription factor NF-κB. c-Abl inhibition might also lead to a dampened ER-stress response, via JNK or other pathways. Inhibition of PDGFR could contribute to decreasing peripheral insulin resistance and inflammatory processes, thereby promoting ß-cell survival. Moreover, inhibition of c-Kit and DDR1/2 might also add to the anti-diabetic effects of imatinib, possibly by interfering with inflammatory responses.
It appears that the four known targets of Imatinib, c-Abl, PDGFR, c-Kit and DDR1/2, may all play a role in the pathogenesis of diabetes. C-Abl is a proapoptotic tyrosine kinase that promotes ß-cell death when activated. Improper activation of the PDGF receptor has also been reported to occur in diabetes, and this may lead to increased insulin resistance of peripheral tissues. Activation of c-Kit and DDR1/2 is known to affect innate immunity, a component of the immune system that promotes inflammation and ß-cell dysfunction. Thus, it is conceivable that Imatinib, by targeting several pathways simultaneously, mediates a stronger antidiabetic effect than other drugs that affect only one particular pathway.
It is the aim of this project to elucidate closer the mechanisms by which tyrosine kinases control ß-cell death and function. We are currently investigating Imatinib-mediated control of NF-κB, JNK, p38, PI3-kinase, SHIP2, PTEN, FAK, IRS1/2, ß-catenin, AKT and ERK signaling events. For this purpose insulin producing cells, either at basal conditions or under stress, are analyzed by immunoprecipitation, immunoblotting, confocal microscopy, real-time PCR, microarray analysis, flow cytometry and gel shift analysis. Cells are also genetically manipulated by lentiviral vectors to achieve up-or down-regulation of specific gene products. Signaling events will be correlated to ß-cell survival and function, as assessed by analysis of insulin production and apoptotic events. This will hopefully lead to a better understanding of the molecular events by which Imatinib protects against diabetes. Such improved knowledge may pave the way for a novel and improved treatment of diabetes.
Role of ROS producing NADPH-dependent oxidases (NOX) in β-cell dysfunction
Loss of pancreatic islet function is a central hallmark in the pathogenesis of T2DM. In addition, it may be that also β-cell loss occurs in T2DM, and that this starts, after an initial phase of hyperinsulinemia, relatively late in the progression of the disease. The mechanisms resulting in beta cell failure in T2DM are not clear, but accumulating evidence point to a central role of oxidative stress as a result of overproduction of reactive oxygen species (ROS) (Figure 1).
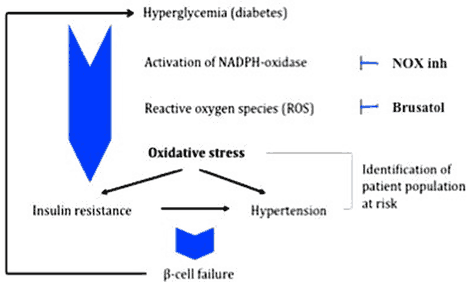
The excessive production and accumulation of ROS is, at least in part, due to hyperactivity of the NADPH oxidases (NOX). The NOX family consists of seven isoforms (NOX1-5 and DUOX1-2), which perform normal cellular functions at basal conditions, but when persistently activated produce harmful levels of ROS. Hyperactivity of some of the isoforms has been found to be an important driver in a number of diseases including diabetes and diabetes complications [11]. The present project will explore ways to protect against β-cell oxidative stress and deterioration by inhibiting NOX, and to define T2DM patient groups that would particularly benefit from treatment with such inhibitors. Novel NOX inhibitors are available to us via Glucox Biotech, a company that possess fundamental patents, granted in the US and in Europe and pending in Japan, which cover the rights to develop anti-diabetes drugs aimed to inhibit NOX. Glucox Biotech also owns international (PCT) substance patent applications on its first and second compound generation.
Reference:
Anvari E, Wikström P, Walum E, Welsh N. The novel NADPH oxidase 4 inhibitor GLX351322 counteracts glucose intolerance in high-fat diet-treated C57BL/6 mice. Free Radic Res. 2015;49(11):1308-18.
Publications
Part of International Journal of Molecular Sciences, 2024
- DOI for GDF15 Protects Insulin-Producing Beta Cells against Pro-Inflammatory Cytokines and Metabolic Stress via Increased Deamination of Intracellular Adenosine
- Download full text (pdf) of GDF15 Protects Insulin-Producing Beta Cells against Pro-Inflammatory Cytokines and Metabolic Stress via Increased Deamination of Intracellular Adenosine
CLEC11A improves insulin secretion and promotes cell proliferation in human beta-cells
Part of Journal of Molecular Endocrinology, 2023
- DOI for CLEC11A improves insulin secretion and promotes cell proliferation in human beta-cells
- Download full text (pdf) of CLEC11A improves insulin secretion and promotes cell proliferation in human beta-cells
Part of Frontiers in Endocrinology, 2023
- DOI for Metabolic stress-induced human beta-cell death is mediated by increased intracellular levels of adenosine
- Download full text (pdf) of Metabolic stress-induced human beta-cell death is mediated by increased intracellular levels of adenosine
Part of Free radical research, p. 460-469, 2023
- DOI for The selective NOX4 inhibitor GLX7013159 decreases blood glucose concentrations and human beta-cell apoptotic rates in diabetic NMRI nu/nu mice transplanted with human islets
- Download full text (pdf) of The selective NOX4 inhibitor GLX7013159 decreases blood glucose concentrations and human beta-cell apoptotic rates in diabetic NMRI nu/nu mice transplanted with human islets
Are off-target effects of imatinib the key to improving beta-cell function in diabetes?
Part of Upsala Journal of Medical Sciences, 2022
- DOI for Are off-target effects of imatinib the key to improving beta-cell function in diabetes?
- Download full text (pdf) of Are off-target effects of imatinib the key to improving beta-cell function in diabetes?
Pharmacological Inhibition of NOX4 Improves Mitochondrial Function and Survival in Human Beta-Cells
Part of Biomedicines, 2021
- DOI for Pharmacological Inhibition of NOX4 Improves Mitochondrial Function and Survival in Human Beta-Cells
- Download full text (pdf) of Pharmacological Inhibition of NOX4 Improves Mitochondrial Function and Survival in Human Beta-Cells
Part of Diabetologia, p. 2292-2305, 2021
- DOI for ZBED6 counteracts high-fat diet-induced glucose intolerance by maintaining beta cell area and reducing excess mitochondrial activation
- Download full text (pdf) of ZBED6 counteracts high-fat diet-induced glucose intolerance by maintaining beta cell area and reducing excess mitochondrial activation
Part of Clinical Science, p. 2243-2263, 2021
The importance of the ZBED6-IGF2 axis for metabolic regulation in mouse myoblast cells
Part of The FASEB Journal, p. 10250-10266, 2020
- DOI for The importance of the ZBED6-IGF2 axis for metabolic regulation in mouse myoblast cells
- Download full text (pdf) of The importance of the ZBED6-IGF2 axis for metabolic regulation in mouse myoblast cells
Part of The FASEB Journal, p. 88-100, 2019
Part of The FASEB Journal, p. 3510-3522, 2019
Part of Proceedings of the National Academy of Sciences of the United States of America, 2018
The novel NADPH oxidase 4 selective inhibitor GLX7013114 counteracts human islet cell death in vitro
Part of PLOS ONE, 2018
- DOI for The novel NADPH oxidase 4 selective inhibitor GLX7013114 counteracts human islet cell death in vitro
- Download full text (pdf) of The novel NADPH oxidase 4 selective inhibitor GLX7013114 counteracts human islet cell death in vitro
Part of Islets, p. 43-48, 2017
Department of Medical Cell Biology: Annual Report 2016
Uppsala University, 2017
Part of Upsala Journal of Medical Sciences, p. 149-159, 2017
- DOI for Addition of exogenous sodium palmitate increases the IAPP/insulin mRNA ratio via GPR40 in human EndoC-beta H1 cells
- Download full text (pdf) of Addition of exogenous sodium palmitate increases the IAPP/insulin mRNA ratio via GPR40 in human EndoC-beta H1 cells
Part of Diabetologia, 2016
Imatinib prevents beta cell death in vitro but does not improve islet transplantation outcome
Part of Upsala Journal of Medical Sciences, p. 140-145, 2016
- DOI for Imatinib prevents beta cell death in vitro but does not improve islet transplantation outcome
- Download full text (pdf) of Imatinib prevents beta cell death in vitro but does not improve islet transplantation outcome
Department of Medical Cell Biology: Annual Report 2015
Uppsala University, 2016
Part of Heliyon, 2016
- DOI for PTB and TIAR binding to insulin mRNA 3'- and 5'UTRs; implications for insulin biosynthesis and messenger stability.
- Download full text (pdf) of PTB and TIAR binding to insulin mRNA 3'- and 5'UTRs; implications for insulin biosynthesis and messenger stability.
Part of European Journal of Pharmacology, p. 69-80, 2016
Part of Scientific Reports, 2016
- DOI for Knock-down of ZBED6 in insulin-producing cells promotes N-cadherin junctions between beta-cells and neural crest stem cells in vitro
- Download full text (pdf) of Knock-down of ZBED6 in insulin-producing cells promotes N-cadherin junctions between beta-cells and neural crest stem cells in vitro
Part of Upsala Journal of Medical Sciences, p. 40-46, 2015
Part of Clinical Science, p. 17-28, 2015
Part of Free radical research, p. 1308-1318, 2015
- DOI for The novel NADPH oxidase 4 inhibitor GLX351322 counteracts glucose intolerance in high-fat diet-treated C57BL/6 mice
- Download full text (pdf) of The novel NADPH oxidase 4 inhibitor GLX351322 counteracts glucose intolerance in high-fat diet-treated C57BL/6 mice
Brusatol inhibits the response of cultured beta-cells to pro-inflammatory cytokines in vitro
Part of Biochemical and Biophysical Research Communications - BBRC, p. 868-872, 2015
- DOI for Brusatol inhibits the response of cultured beta-cells to pro-inflammatory cytokines in vitro
- Download full text (pdf) of Brusatol inhibits the response of cultured beta-cells to pro-inflammatory cytokines in vitro
Department of Medical Cell Biology: Annual Report 2014
Uppsala universitet, 2015
Role of the AMP kinase in cytokine-induced human EndoC-beta H1 cell death
Part of Molecular and Cellular Endocrinology, p. 53-63, 2015
- DOI for Role of the AMP kinase in cytokine-induced human EndoC-beta H1 cell death
- Download full text (pdf) of Role of the AMP kinase in cytokine-induced human EndoC-beta H1 cell death
Activated pancreatic stellate cells can impair pancreatic islet function in mice
Part of Upsala Journal of Medical Sciences, p. 169-180, 2015
Part of Pancreas, p. 624-629, 2014
Part of Upsala Journal of Medical Sciences, p. 306-315, 2014
- DOI for Bcl-2 maintains the mitochondrial membrane potential, but fails to affect production of reactive oxygen species and endoplasmic reticulum stress, in sodium palmitate-induced beta-cell death
- Download full text (pdf) of Bcl-2 maintains the mitochondrial membrane potential, but fails to affect production of reactive oxygen species and endoplasmic reticulum stress, in sodium palmitate-induced beta-cell death
Part of Genomics, p. 264-275, 2014
Part of Transplantation, 2013
Part of Diabetologia, p. 1327-1338, 2013
- DOI for Imatinib mesilate-induced phosphatidylinositol 3-kinase signalling and improved survival in insulin-producing cells: role of Src homology 2-containing inositol 5'-phosphatase interaction with c-Abl
- Download full text (pdf) of Imatinib mesilate-induced phosphatidylinositol 3-kinase signalling and improved survival in insulin-producing cells: role of Src homology 2-containing inositol 5'-phosphatase interaction with c-Abl
Part of PLOS ONE, 2013
- DOI for Co-Culture of Neural Crest Stem Cells (NCSC) and Insulin Producing Beta-TC6 Cells Results in Cadherin Junctions and Protection against Cytokine-Induced Beta-Cell Death
- Download full text (pdf) of Co-Culture of Neural Crest Stem Cells (NCSC) and Insulin Producing Beta-TC6 Cells Results in Cadherin Junctions and Protection against Cytokine-Induced Beta-Cell Death
Part of Proceedings of the National Academy of Sciences of the United States of America, p. 15997-16002, 2013
Part of Cell Death and Differentiation, p. 1836-1846, 2012
Part of Pancreas, p. 490-492, 2012
Part of Biochemical and Biophysical Research Communications - BBRC, p. 845-850, 2012
- DOI for Cytokine-induced human islet cell death in vitro correlateswith a persistently high phosphorylation of STAT-1, but not with NF-κB activation
- Download full text (pdf) of Cytokine-induced human islet cell death in vitro correlateswith a persistently high phosphorylation of STAT-1, but not with NF-κB activation
Part of Expert Opinion on Investigational Drugs, p. 1743-1750, 2012
- DOI for Does the small tyrosine kinase inhibitor imatinib mesylate counteract diabetes by affecting pancreatic islet amyloidosis and fibrosis?
- Download full text (pdf) of Does the small tyrosine kinase inhibitor imatinib mesylate counteract diabetes by affecting pancreatic islet amyloidosis and fibrosis?
The human insulin mRNA is partly translated via a cap- and eIF4A-independent mechanism
Part of Biochemical and Biophysical Research Communications - BBRC, p. 693-698, 2011
Part of PLOS ONE, 2011
Part of PLOS ONE, 2010
Part of Textbook of Diabetes, p. 1064-1069, Wiley-Blackwell, 2010
Potential utility of small tyrosine kinase inhibitors in the treatment of diabetes
Part of Clinical Science, p. 241-247, 2010
Part of Biochemical and Biophysical Research Communications - BBRC, p. 553-557, 2009
The importance of RNA binding proteins in preproinsulin mRNA stability
Part of Molecular and Cellular Endocrinology, p. 28-33, 2009
Part of American Journal of Physiology. Endocrinology and Metabolism, 2009
Detailed transcriptome atlas of the pancreatic beta cell
Part of BMC Medical Genomics, p. 3, 2009
Part of Biochemical Pharmacology, p. 1748-1756, 2008

