Per-Ola Carlsson
Beta cell therapy and regenerative medicine
The overall aim of the research group is to develop means to intervene with the development of type 1 diabetes mellitus and find treatment strategies to restore glucose homeostasis in patients with type 1 diabetes mellitus using cell therapy and regenerative medicine.
The dual role of the P.I. Per-Ola Carlsson as experimental and clinical scientist simplifies translational approaches, and the research group is active both at the Department of Medical Cell Biology and the Department of Medical Sciences. Studies are conducted to elucidate the importance of islet endothelial, neural, stromal or their progenitor cells for beta-cell regeneration and function, and to investigate the concept of islet heterogeneity. Other studies investigate the adaptation of pancreatic islets and stem-cell derived beta-cells to the implantation organ, i.e. the so called engraftment process, following transplantation, and develop bioengineering strategies (coating of islets with supporting stem cells, oxygen carriers and growth factors, as well as with use of scaffolds) to improve results by enhancement of engraftment e.g. by improved revascularization. Human beta-cells are tested in these experimental systems with a focus to produce clinically applicable protocols.
We also perform research to develop safe and effective means to generate new human beta-cells by stimulating adult beta-cell proliferation, e.g. by stem cell stimulation, or by stem cell differentiation. Clinical studies are performed to prevent development of type 1 diabetes in patients, e.g. by mesenchymal stem cell therapy, and to develop means for beta-cell imaging by positron emission tomography. We also conduct studies to improve the results of clinical beta-cells replacement, e.g. by encapsulation in order to avoid immune suppression of the patients.
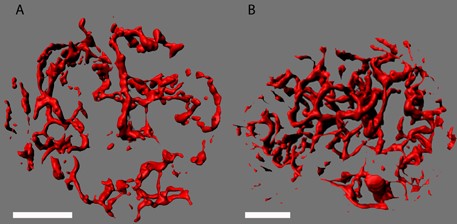
Fig 1. Two-photon confocal images of vascularity in pancreatic islets with low (A) or high (B) blood perfusion (blood perfusion identified by microsphere measurements).
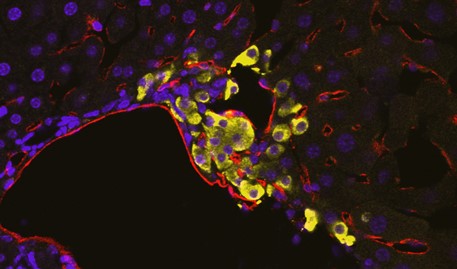
Fig 2. Micrograph showing vascularization of intraportally transplanted islet with disrupted integrity in the wall of a portal vein tributary. Yellow depicts insulin; red CD31 staining for blood vessels and blue DAPI.
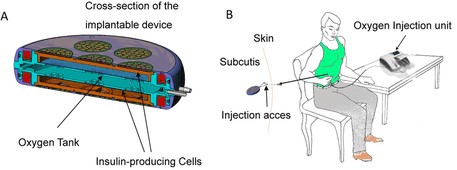
Fig 3. Macroencapsulation of insulin-producing cells in the oxygenated Beta-Air device for treatment in type 1 diabetes (A). Device implanted subcutaneously and oxygen tank refilled once daily through the injection ports (B).
For further information about this research group please contact
Professor Per-Ola Carlsson: Per-Ola.Carlsson@mcb.uu.se
Publications
Predictive biomarkers of rapidly developing insulin deficiency in children with type 1 diabetes
Part of BMJ Open Diabetes Research & Care, 2024
- DOI for Predictive biomarkers of rapidly developing insulin deficiency in children with type 1 diabetes
- Download full text (pdf) of Predictive biomarkers of rapidly developing insulin deficiency in children with type 1 diabetes
Part of Cell Stem Cell, p. 38-51, 2023
- DOI for An insulin hypersecretion phenotype precedes pancreatic beta cell failure in MODY3 patient-specific cells
- Download full text (pdf) of An insulin hypersecretion phenotype precedes pancreatic beta cell failure in MODY3 patient-specific cells
Part of Diabetologia, p. 1431-1441, 2023
- DOI for Umbilical cord-derived mesenchymal stromal cells preserve endogenous insulin production in type 1 diabetes: a Phase I/II randomised double-blind placebo-controlled trial
- Download full text (pdf) of Umbilical cord-derived mesenchymal stromal cells preserve endogenous insulin production in type 1 diabetes: a Phase I/II randomised double-blind placebo-controlled trial
Classification of Hypoglycemic Events in Type 1 Diabetes Using Machine Learning Algorithms
Part of Diabetes Therapy, p. 953-965, 2023
Part of Free radical research, p. 460-469, 2023
- DOI for The selective NOX4 inhibitor GLX7013159 decreases blood glucose concentrations and human beta-cell apoptotic rates in diabetic NMRI nu/nu mice transplanted with human islets
- Download full text (pdf) of The selective NOX4 inhibitor GLX7013159 decreases blood glucose concentrations and human beta-cell apoptotic rates in diabetic NMRI nu/nu mice transplanted with human islets
Part of Biomedicines, 2022
- DOI for Endogenous Levels of Gamma Amino-Butyric Acid Are Correlated to Glutamic-Acid Decarboxylase Antibody Levels in Type 1 Diabetes
- Download full text (pdf) of Endogenous Levels of Gamma Amino-Butyric Acid Are Correlated to Glutamic-Acid Decarboxylase Antibody Levels in Type 1 Diabetes
Pregnancy induces pancreatic insulin secretion in women with long-standing type 1 diabetes
Part of BMJ Open Diabetes Research & Care, 2022
- DOI for Pregnancy induces pancreatic insulin secretion in women with long-standing type 1 diabetes
- Download full text (pdf) of Pregnancy induces pancreatic insulin secretion in women with long-standing type 1 diabetes
Part of Nature Biotechnology, p. 1042-1055, 2022
- DOI for Functional, metabolic and transcriptional maturation of human pancreatic islets derived from stem cells.
- Download full text (pdf) of Functional, metabolic and transcriptional maturation of human pancreatic islets derived from stem cells.
Part of BMJ Open Diabetes Research & Care, 2022
- DOI for Higher risk of severe hypoglycemia in children and adolescents with a rapid loss of C-peptide during the first 6 years after type 1 diabetes diagnosis
- Download full text (pdf) of Higher risk of severe hypoglycemia in children and adolescents with a rapid loss of C-peptide during the first 6 years after type 1 diabetes diagnosis
Part of Pediatric Diabetes, p. 341-350, 2022
- DOI for Good glycemic control without exceeding the BMI trajectory during the first 5 years of treatment in children and adolescents with type 1 diabetes
- Download full text (pdf) of Good glycemic control without exceeding the BMI trajectory during the first 5 years of treatment in children and adolescents with type 1 diabetes
Irisin-A Pancreatic Islet Hormone
Part of Biomedicines, 2022
- DOI for Irisin-A Pancreatic Islet Hormone
- Download full text (pdf) of Irisin-A Pancreatic Islet Hormone
Part of Obesity, p. 535-542, 2021
- DOI for Changes in Circulating Cytokines and Adipokines After RYGB in Patients with and without Type 2 Diabetes
- Download full text (pdf) of Changes in Circulating Cytokines and Adipokines After RYGB in Patients with and without Type 2 Diabetes
Longitudinal Assessment of 11C-5-Hydroxytryptophan Uptake in Pancreas After Debut of Type 1 Diabetes
Part of Diabetes, p. 966-975, 2021
Potential of [C-11]UCB-J as a PET tracer for islets of Langerhans
Part of Scientific Reports, 2021
- DOI for Potential of [C-11]UCB-J as a PET tracer for islets of Langerhans
- Download full text (pdf) of Potential of [C-11]UCB-J as a PET tracer for islets of Langerhans
Part of Stem Cell Research, 2021
- DOI for Generation of human induced pluripotent stem cell (iPSC) lines (UUMCBi001-A, UUMCBi002-A) from two healthy donors
- Download full text (pdf) of Generation of human induced pluripotent stem cell (iPSC) lines (UUMCBi001-A, UUMCBi002-A) from two healthy donors
GABA induces a hormonal counter-regulatory response in subjects with long-standing type 1 diabetes
Part of BMJ Open Diabetes Research & Care, 2021
- DOI for GABA induces a hormonal counter-regulatory response in subjects with long-standing type 1 diabetes
- Download full text (pdf) of GABA induces a hormonal counter-regulatory response in subjects with long-standing type 1 diabetes
Pharmacological Inhibition of NOX4 Improves Mitochondrial Function and Survival in Human Beta-Cells
Part of Biomedicines, 2021
- DOI for Pharmacological Inhibition of NOX4 Improves Mitochondrial Function and Survival in Human Beta-Cells
- Download full text (pdf) of Pharmacological Inhibition of NOX4 Improves Mitochondrial Function and Survival in Human Beta-Cells
Part of International Journal of Molecular Sciences, 2021
- DOI for Interleukin-35 Prevents Development of Autoimmune Diabetes Possibly by Maintaining the Phenotype of Regulatory B Cells
- Download full text (pdf) of Interleukin-35 Prevents Development of Autoimmune Diabetes Possibly by Maintaining the Phenotype of Regulatory B Cells
Function and Gene Expression of Islets Experimentally Transplanted to Muscle and Omentum
Part of Cell Transplantation, p. 1-10, 2020
- DOI for Function and Gene Expression of Islets Experimentally Transplanted to Muscle and Omentum
- Download full text (pdf) of Function and Gene Expression of Islets Experimentally Transplanted to Muscle and Omentum
Part of Physiological Reports, 2020
- DOI for Highly blood perfused, highly metabolically active pancreatic islets may be more susceptible for immune attack
- Download full text (pdf) of Highly blood perfused, highly metabolically active pancreatic islets may be more susceptible for immune attack
Part of Journal of Clinical Endocrinology and Metabolism, 2020
- DOI for Physical Activity, Genetic Susceptibility, and the Risk of Latent Autoimmune Diabetes in Adults and Type 2 Diabetes
- Download full text (pdf) of Physical Activity, Genetic Susceptibility, and the Risk of Latent Autoimmune Diabetes in Adults and Type 2 Diabetes
Part of BMJ Open Diabetes Research & Care, 2020
- DOI for Better HbA1c during the first years after diagnosis of type 1 diabetes is associated with residual C peptide 10 years later
- Download full text (pdf) of Better HbA1c during the first years after diagnosis of type 1 diabetes is associated with residual C peptide 10 years later
Part of Frontiers in Immunology, 2020
- DOI for Increased Plasma Levels of the Co-stimulatory Proteins CDCP1 and SLAMF1 in Patients With Autoimmune Endocrine Diseases
- Download full text (pdf) of Increased Plasma Levels of the Co-stimulatory Proteins CDCP1 and SLAMF1 in Patients With Autoimmune Endocrine Diseases
Part of Frontiers in Immunology, 2020
- DOI for Mass Cytometry Studies of Patients With Autoimmune Endocrine Diseases Reveal Distinct Disease-Specific Alterations in Immune Cell Subsets
- Download full text (pdf) of Mass Cytometry Studies of Patients With Autoimmune Endocrine Diseases Reveal Distinct Disease-Specific Alterations in Immune Cell Subsets
Part of Experimental Cell Research, p. 1-8, 2019
Part of Clinical and Experimental Immunology, p. 64-73, 2019
- DOI for Cellular immunological changes in patients with LADA are a mixture of those seen in patients with type 1 and type 2 diabetes
- Download full text (pdf) of Cellular immunological changes in patients with LADA are a mixture of those seen in patients with type 1 and type 2 diabetes
A modified in vitro tool for isolation and characterization of rat quiescent islet stellate cells
Part of Experimental Cell Research, 2019
Part of Cell Transplantation, p. 1455-1460, 2019
- DOI for Fewer Islets Survive from a First Transplant than a Second Transplant: Evaluation of Repeated Intraportal Islet Transplantation in Mice
- Download full text (pdf) of Fewer Islets Survive from a First Transplant than a Second Transplant: Evaluation of Repeated Intraportal Islet Transplantation in Mice
Pancreatic Blood Flow with Special Emphasis on Blood Perfusion of the Islets of Langerhans
Part of COMPREHENSIVE PHYSIOLOGY, p. 799-837, 2019
Ghrelin in rat pancreatic islets decreases islet blood flow
Part of American Journal of Physiology. Endocrinology and Metabolism, 2019
Part of Journal of the Endocrine Society, p. 1608-1616, 2019
- DOI for Decreased beta-Cell Proliferation and Vascular Density in a Subpopulation of Low-Oxygenated Male Rat Islets
- Download full text (pdf) of Decreased beta-Cell Proliferation and Vascular Density in a Subpopulation of Low-Oxygenated Male Rat Islets
Unsurpassed Intrahepatic Islet Engraftment: the Quest for New Sites for Beta Cell Replacement
Part of Cell Medicine, 2019
- DOI for Unsurpassed Intrahepatic Islet Engraftment: the Quest for New Sites for Beta Cell Replacement
- Download full text (pdf) of Unsurpassed Intrahepatic Islet Engraftment: the Quest for New Sites for Beta Cell Replacement
Part of Diabetologia, p. 896-905, 2018
- DOI for Early deficits in insulin secretion, beta cell mass and islet blood perfusion precede onset of autoimmune type 1 diabetes in BioBreeding rats
- Download full text (pdf) of Early deficits in insulin secretion, beta cell mass and islet blood perfusion precede onset of autoimmune type 1 diabetes in BioBreeding rats
Part of Diabetologia, p. 1333-1343, 2018
- DOI for Overweight, obesity and the risk of LADA: results from a Swedish case-control study and the Norwegian HUNT Study
- Download full text (pdf) of Overweight, obesity and the risk of LADA: results from a Swedish case-control study and the Norwegian HUNT Study
Ghrelin in rat pancreatic islets decreases islet blood flow and impairs insulin secretion
Part of Diabetologia, 2018
Part of Diabetes & Metabolism, p. 354-360, 2018
Part of European Journal of Clinical Investigation, p. 83-83, 2018
Part of American Journal of Transplantation, p. 1735-1744, 2018
- DOI for Transplantation of macroencapsulated human islets within the bioartificial pancreas βAir to patients with type 1 diabetes mellitus
- Download full text (pdf) of Transplantation of macroencapsulated human islets within the bioartificial pancreas βAir to patients with type 1 diabetes mellitus
Part of Cell Transplantation, p. 948-956, 2018
- DOI for Bioengineering with Endothelial Progenitor Cells Improves the Vascular Engraftment of Transplanted Human Islets
- Download full text (pdf) of Bioengineering with Endothelial Progenitor Cells Improves the Vascular Engraftment of Transplanted Human Islets
Part of EBioMedicine, p. 283-294, 2018
- DOI for GABA Regulates Release of Inflammatory Cytokines From Peripheral Blood Mononuclear Cells and CD4+ T Cells and Is Immunosuppressive in Type 1 Diabetes
- Download full text (pdf) of GABA Regulates Release of Inflammatory Cytokines From Peripheral Blood Mononuclear Cells and CD4+ T Cells and Is Immunosuppressive in Type 1 Diabetes
Functional Characterization of Native, High-Affinity GABAA Receptors in Human Pancreatic β Cells
Part of EBioMedicine, 2018
- DOI for Functional Characterization of Native, High-Affinity GABAA Receptors in Human Pancreatic β Cells
- Download full text (pdf) of Functional Characterization of Native, High-Affinity GABAA Receptors in Human Pancreatic β Cells
Non-lab and semi-lab algorithms for screening undiagnosed diabetes: A cross-sectional study
Part of EBioMedicine, p. 307-316, 2018
- DOI for Non-lab and semi-lab algorithms for screening undiagnosed diabetes: A cross-sectional study
- Download full text (pdf) of Non-lab and semi-lab algorithms for screening undiagnosed diabetes: A cross-sectional study
Part of PLOS ONE, 2018
- DOI for Expression of calcium release-activated and voltage-gated calcium channels genes in peripheral blood mononuclear cells is altered in pregnancy and in type 1 diabetes
- Download full text (pdf) of Expression of calcium release-activated and voltage-gated calcium channels genes in peripheral blood mononuclear cells is altered in pregnancy and in type 1 diabetes
The novel NADPH oxidase 4 selective inhibitor GLX7013114 counteracts human islet cell death in vitro
Part of PLOS ONE, 2018
- DOI for The novel NADPH oxidase 4 selective inhibitor GLX7013114 counteracts human islet cell death in vitro
- Download full text (pdf) of The novel NADPH oxidase 4 selective inhibitor GLX7013114 counteracts human islet cell death in vitro
Increased Interleukin-35 Levels in Patients With Type 1 Diabetes With Remaining C-Peptide
Part of Diabetes Care, p. 1090-1095, 2017
Part of Diabetic Medicine, p. 514-521, 2017
[(11)C]5-Hydroxy-Tryptophan PET for Assessment of Islet Mass During Progression of Type 2 Diabetes
Part of Diabetes, p. 1286-1292, 2017
Family history of type 1 and type 2 diabetes and risk of latent autoimmune diabetes in adults (LADA)
Part of Diabetes & Metabolism, p. 536-542, 2017
Towards the clinical translation of stem cell therapy for type 1 diabetes
Part of European Journal of Endocrinology, 2017
Role of regulatory B cells in clinical and experimental type 1 diabetes
Part of Scandinavian Journal of Immunology, p. 349-349, 2017

