Evaluating the utility and use of existing tools to optimize antibiotic prescription in India
Antibiotic resistance (ABR) is one of the greatest threats to health and sustainable development. India is the world’s greatest consumer of antibiotics. and all use of antibiotics promotes the development of resistance. Diagnostics are one of the tools which could transform the way we prescribe antibiotics in healthcare. To improve access to diagnostics to combat ABR in LMICs, the WHO recommends better use of existing diagnostics. Diagnostic tools must be useful to healthcare providers and beneficial for patients in the defined site of use. Their utility for diagnosis of bacterial infection in the defined population and site of use must be established. Informed strategies to implement their use are necessary to ensure their adoption into sustainable clinical practice.
C-Reactive Protein (CRP) is the most promising biomarker test in the literature that can be used to determine if an infection is of bacterial aetiology and could be feasible for use in LMICs. Cut-off levels indicating infections of bacterial aetiology can vary due to comorbidities such as malaria, HIV and malnutrition and the stage of disease presentation. To increase the utility and safely be able to use CRP in India, it is essential to evaluate its performance in distinguishing between bacterial and non-bacterial infections, and appropriate cut-off levels must be set. Furthermore, if we aim to support the adoption of diagnostics into sustainable practice, guidance is needed on how to develop contextually tailored implementation strategies.

Bronwen and collaborators working on site in Ujjain, India.
The overall aim of the PhD project is to improve access to existing diagnostics to combat antibiotic resistance, by increasing the evidence-base on the utility and use of existing diagnostics to distinguish bacterial from non-bacterial causes of fever to optimize antibiotic prescription in outpatients in Ujjain, India. The specific objectives (and related methods) are:
STUDY I: To investigate the utilization of existing diagnostics by caregivers of sick children attending the paediatric outpatient department at a tertiary hospital (interviews and observations);
STUDY II: To determine the etiology of non-severe febrile illness (prospective case series, laboratory methods combined with expert clinical assessment to classify the infection);
STUDY III: To evaluate the performance characteristics and establish appropriate cut-offs for CRP as a biomarker to aid in differentiating bacterial from non-bacterial infections in febrile children and adults (calculate sensitivity and specificity of CRP based on expert classification and CRP values);
STUDY IV: To evaluate the utility of CRP to improve antibiotic prescription for acute febrile children and adults (a retrospective correlation of provisional diagnosis and antibiotic prescription made by the residents with the CRP test results and cut-off levels established in Study III)
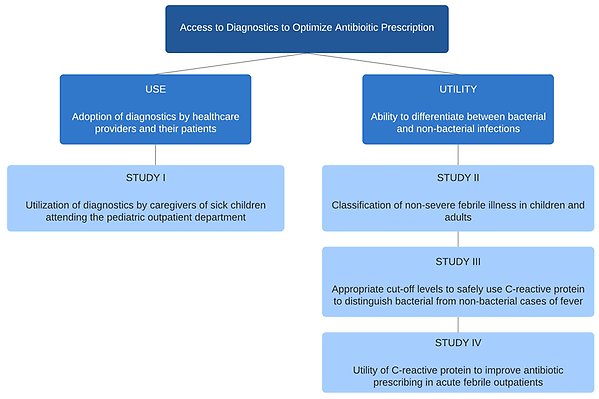
Conceptual framework of this study
Related published research
- Blacklock C, Gonçalves Bradley DC, Mickan S, Willcox M, Roberts N, Bergström A, et al. Impact of Contextual Factors on the Effect of Interventions to Improve Health Worker Performance in Sub-Saharan Africa: Review of Randomised Clinical Trials. PLoS ONE, 2016. 11(1): e0145206
- Duong DM, Bergström A, Wallin L, Bui HT, Eriksson L, Eldh AC. Exploring the influence of context in a community-based facilitation intervention focusing on neonatal health and survival in Vietnam: a qualitative study. BMC Public Health, 2015. 15(1): p. 814.
- Pathak A, Mahadik K, Dhaneria SP, Sharma A, Eriksson B, Lundborg CS. Antibiotic prescribing in outpatients: Hospital and seasonal variations in Ujjain, India. Scand J Infect Dis. 2011 Jul;43(6–7):479–88.
- Sharma M, Damlin A, Pathak A, Stålsby Lundborg C. Antibiotic Prescribing among Pediatric Inpatients with Potential Infections in Two Private Sector Hospitals in Central India. PloS One. 2015;10(11):e0142317.
- Rhedin SA, Eklundh A, Ryd-Rinder M, Naucler P, Mårtensson A, Gantelius J, Zenk I, Andersson-Svahn H, Nybond S, Rasti R, Lindh M, Andersson M, Peltola V, Waris M, Alfvén T. Introducing a New Algorithm for Classification of Etiology in Studies on Pediatric Pneumonia: Protocol for the Trial of Respiratory Infections in Children for Enhanced Diagnostics Study. JMIR Res Protoc. 2019 Apr 26;8(4):e12705.
- Andersson M, Kabayiza JC, Elfving K, Nilsson S, Msellem MI, Mårtensson A, Björkman A, Bergström T, Lindh M., Coinfection with Enteric Pathogens in East African Children with Acute Gastroenteritis-Associations and Interpretations. Am J Trop Med Hyg. 2018 Apr 23.
- Katia J. Bruxvoort, Baptiste Leurent, Clare I. R. Chandler, Evelyn K. Ansah, Frank Baiden, Anders Björkman, Helen E. D. Burchett, Sîan E. Clarke, Bonnie Cundill, Debora D. DiLiberto, Kristina Elfving, Catherine Goodman, Kristian S. Hansen, S. Patrick Kachur, Sham Lal, David G. Lalloo, Toby Leslie, Pascal Magnussen, Lindsay Mangham-Jefferies, Andreas Mårtensson, Ismail Mayan, Anthony K. Mbonye, Mwinyi I. Msellem, Obinna E. Onwujekwe, Seth Owusu-Agyei, Mark W. Rowland, Delér Shakely, Sarah G. Staedke, Lasse S. Vestergaard, Jayne Webster, Christopher J. M. Whitty, Virginia L. Wiseman, Shunmay Yeung, David Schellenberg and Heidi Hopkins. The Impact of Introducing Malaria Rapid Diagnostic Tests on Fever Case Management: A Synthesis of Ten Studies from the ACT Consortium. American Journal of Tropical Medicine and Hygiene. Available online: 07 August 2017.
- Rasti R, Nanjebe D, Karlström J, Muchunguzi C, Mwanga-Amumpaire J, Gantelius J, Mårtensson A, Rivas L, Galban F, Reuterswärd P, Andersson Svahn H, Alvesson HM, Boum Y 2nd, Alfvén T. Health care workers' perceptions of point-of-care testing in a low-income country -A qualitative study in Southwestern Uganda. PLoS One. 2017 Jul 27;12(7):e0182005. doi: 10.1371/journal.pone.0182005. eCollection 2017.
- Burchett HE, Leurent B, Baiden F, Baltzell K, Björkman A, Bruxvoort K. Clarke S, DiLiberto D, Elfving K, Goodman C, Hopkins H, Lal S, Liverani M, Magnussen P, Mårtensson A, Mbacham W, Mbonye A, Onwujekwe O, Roth Allen D, Shakely D, Staedke S, Vestergaard LS, Whitty CJ, Wiseman V, Chandler CI. Improving prescribing practices with rapid diagnostic tests (RDTs): synthesis of 10 studies to explore reasons for variation in malaria RDT uptake and adherence. BMJ Open. 2017 Mar 8;7(3):e012973.
- Elfving K, Shakely D, Andersson M, Baltzell K, Ali AS, Bachelard M, Falk KI, Ljung A, Msellem MI, Omar RS, Parola P, Xu W, Petzold M, Trollfors B, Björkman A, Lindh M, Mårtensson A. Acute Uncomplicated Febrile Illness in Children Aged 2-59 months in Zanzibar - Aetiologies, Antibiotic Treatment and Outcome. PLoS One. 2016 Jan 28;11(1):e0146054
