Systematic mapping of antibiotic usage patterns among sick children across low- and middle-income countries from 2005–2017 and its health system, policy and epidemiology drivers
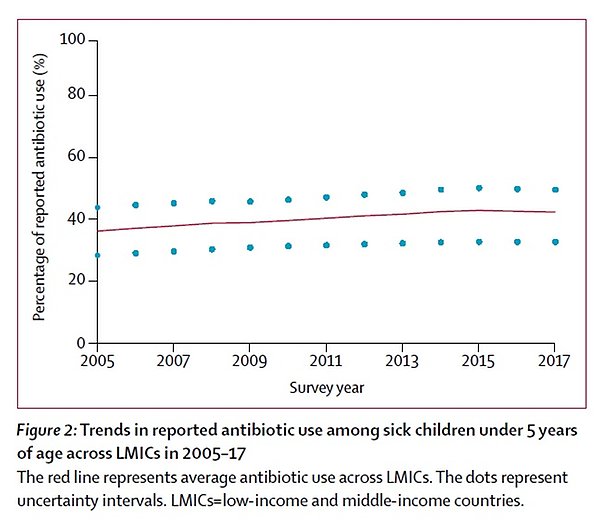
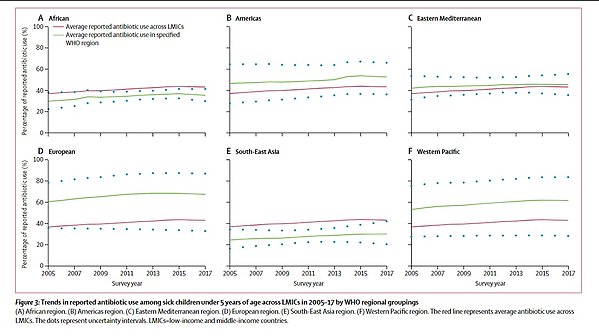
There is a critical need to achieve balance between access to and excess use of antibiotic medicines in order to combat resistance, one of today’s top global health challenges. While high-income countries must limit excess antibiotic use, millions of people worldwide lack access to life-saving medicines. Yet, it is increasingly recognized that the access-excess divide in antibiotic consumption is more complicated than simply between rich and poor countries. There are also important geographic and socioeconomic differentials in antibiotic usage across low- and middle-income countries that need to be identified and addressed to reduce access disparities. Previous global antibiotic consumption assessments have primarily relied on pharmaceutical sales data, which were to a large extent from high-income and upper-middle-income countries, with little representation of low-income and lower-middle-income countries. Pharmaceutical sales data also do not directly measure population antibiotic usage or its variations across socioeconomic groups. To fill this evidence gap, this project aims to analyze national population-based surveys comparably conducted across low- and middle-income countries in 2005–2017 to identify global trends, regional variations and socio-economic differentials. These large-scale analyses will be complemented by an in-depth field study on antibiotic stewardship practices in Uganda, a low-income country with high antibiotic use and rising resistance rates. Taken together, project findings will provide new and important evidence of changing antibiotic use patterns for sick children in low- and middle-income countries including key health system, policy or epidemiological drivers.
Related published research
- Anaba, Udochisom, Paul L. Hutchinson, Dele Abegunde, and Emily White Johansson. "Pneumonia-Related Ideations, Care-Seeking, and Treatment Behaviors among Children under 2 Years with Pneumonia Symptoms in Northwestern Nigeria." Pediatric Pulmonology 55, no. S1 (2020): S91-S103.
- Buchner, D. L., F. E. Kitutu, D. E. Cross, E. Nakamoga, and P. Awor. "A Cross-Sectional Study to Identify the Distribution and Characteristics of Licensed and Unlicensed Private Drug Shops in Rural Eastern Uganda to Inform an Iccm Intervention to Improve Health Outcomes for Children under Five Years." PLoS One 14, no. 1 (2019): e0209641.
- Hussain-Alkhateeb, L., A. Kroeger, P. Olliaro, J. Rocklöv, M. O. Sewe, G. Tejeda, D. Benitez, et al. "Early Warning and Response System (Ewars) for Dengue Outbreaks: Recent Advancements Towards Widespread Applications in Critical Settings." [In eng]. PLoS One 13, no. 5 (2018): e0196811.
- Johansson, E. W., H. Nsona, L. Carvajal-Aguirre, A. Amouzou, and H. Hildenwall. "Determinants of Integrated Management of Childhood Illness (Imci) Non-Severe Pneumonia Classification and Care in Malawi Health Facilities: Analysis of a National Facility Census." [In eng]. J Glob Health 7, no. 2 (Dec 2017): 020408.
- Johansson, E. W., K. E. Selling, H. Nsona, B. Mappin, P. W. Gething, M. Petzold, S. S. Peterson, and H. Hildenwall. "Integrated Paediatric Fever Management and Antibiotic over-Treatment in Malawi Health Facilities: Data Mining a National Facility Census." [In eng]. Malar J 15, no. 1 (Aug 4 2016): 396.
- Johansson, Emily White, Freddy Eric Kitutu, Chrispus Mayora, Phyllis Awor, Stefan Swartling Peterson, Henry Wamani, and Helena Hildenwall. "It Could Be Viral but You Don’t Know, You Have Not Diagnosed It: Health Worker Challenges in Managing Non-Malaria Paediatric Fevers in the Low Transmission Area of Mbarara District, Uganda." Malaria Journal 15, no. 1 (2016/04/11 2016): 197.
- Kitutu, F. E., J. N. Kalyango, C. Mayora, K. E. Selling, S. Peterson, and H. Wamani. "Integrated Community Case Management by Drug Sellers Influences Appropriate Treatment of Paediatric Febrile Illness in South Western Uganda: A Quasi-Experimental Study." Malar J 16, no. 1 (Oct 23 2017): 425.
- Kitutu, F. E., H. Wamani, K. E. Selling, F. A. Katabazi, R. B. Kuteesa, S. Peterson, J. N. Kalyango, and A. Mårtensson. "Can Malaria Rapid Diagnostic Tests by Drug Sellers under Field Conditions Classify Children 5 years Old or Less with or without Plasmodium Falciparum Malaria? Comparison with Nested Pcr Analysis." [In eng]. Malar J 17, no. 1 (Oct 16 2018): 365.
- Mayora, C., F. E. Kitutu, N. B. Kandala, E. Ekirapa-Kiracho, S. S. Peterson, and H. Wamani. "Private Retail Drug Shops: What They Are, How They Operate, and Implications for Health Care Delivery in Rural Uganda." [In eng]. BMC Health Serv Res 18, no. 1 (Jul 9 2018): 532.
- Rhedin, Samuel Arthur, Annika Eklundh, Malin Ryd-Rinder, Pontus Naucler, Andreas Mårtensson, Jesper Gantelius, Ingela Zenk, et al. "Introducing a New Algorithm for Classification of Etiology in Studies on Pediatric Pneumonia: Protocol for the Trial of Respiratory Infections in Children for Enhanced Diagnostics Study." [In eng]. JMIR research protocols 8, no. 4 (2019): e12705-e05.
