Maria Ulvmar research group
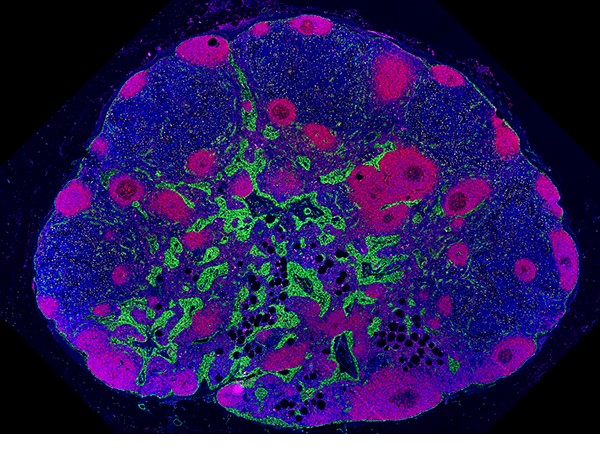
The image shows a human axillary lymph node. B-cells are shown in purple, fibroblastic reticular cells in yellow, and the vasculature in green. This LN is affected by LN lipomatosis seen by the round black dots, interspersed between the normal tissue.
Vascular immunology
My team aims to expand the current knowledge about the lymph node (LN) vascular specialization and plasticity and break new grounds for an understanding of tumour-host communication in the pre-metastatic and the metastatic LN. Our most recent findings and interest also include to understand the implications of age-related changes in the human LN.
The vasculature has long been seen as mainly a conduit for fluid, antigens and immune cells, build up by endothelial cells that were thought to be structurally and molecularly fairly homogenous. Data during the recent years are completely changing this view and show that organ-specific gene expression and functions are common. In this context the lymph nodes (LNs) stand out as having one of the most molecularly complex and versatile vascular beds in our body.
The lymph nodes: central role for induction of immune responses
The LNs are secondary lymphoid organs that are essential for the induction of effective adaptive immune responses in our body. Highly specialized blood and lymphatic vessels determine the entry and the exit of blood respectively tissue-derived immune cell into the LN. While the high endothelial venules (HEVs) recruit naïve T- and B-cells from our blood stream into the LN, the lymphatic vessels make sure that antigen presenting cells from the peripheral tissues find their way to the LN and provide routes out of the LN for activated immune cells. Our research has shown that the lymphatic vessels in the LNs, also directly contribute to immune regulation through the expression of immunomodulatory genes (Ulvmar M.H. et al., 2014, Xiang et al., 2020). Still major questions remains and we are looking forward to new advances to our understanding of organ-specific and immune-regulating functions of the endothelium.
A single-cell transcriptional road-map of the mouse and human lymphatic vasculature
In an international collaboration our lab has mapped the adult human and mouse lymph node (LN) lymphatic endothelial cells (LECs) at the single-cell transcriptional level. In collaboration with Eugene Butcher’s lab we here provide one mouse and one human database resource for academic and other non-commercial purposes, allowing to explore gene expression patterns across LN LECs.
Increased knowledge about regulation of LN immune functions
With our research we want to achieve a better understanding of the basic functions of the LN vasculature and how the vasculature cooperate with other stromal cells and with the immune cells to regulate the LN immune functions. This knowledge can eventually lead to new strategies to improve the immune responses in e.g. vaccination or in immunotherapy. We are also answering how structural and molecular changes of the LN vessels can affect the immune response in cancer disease and the ability of the tumor cells to spread in the body (metastasize). My group address these questions by genetic targeting in mouse models, high parameter flow cytometry and single-cell RNA sequencing but also by studies of human clinical and biobank tissue samples.
The lymph node in cancer disease and aging
The tumor draining LNs are one of the most common and earliest metastatic sites in several human cancer forms, e.g. in breast cancer and pancreatic cancer. We are exploring how tumor drainage and LN metastasis affect the LN vasculature and supporting stromal cells and how these changes can contribute to immunosuppression and metastatic spread in cancer. By identifying pathways that could contribute to sustain tumor growth and vascular interactions in the LN, our research have the potential to eventually lead to new therapeutic strategies to counteract metastasis and promote anti-tumor immune responses. Another reason to study the tumor draining LNs is the potential to find new biomarkers for better prediction of disease progression and/or therapeutic responses in cancer patients. Our work on LNs in cancer is to a large extent focused on human biobank material from patients, complemented by experimental models. We recently also demonstrated that LNs in human develop age-related changes in the form of LN lipomatosis (where fat exchanges the normal tissue). To understand how this affects the immune functions of the LN, is another goal for our work. To analyze human tissue we need to find new solutions for high throughput automated image analysis. The HEV-finder is one of our recent tools for AI-driven automatic analysis of specialized blood vessels in the LN. Recent papers describing our work on human LNs includes:
Twitter: @ulvmar_maria
Maria Ulvmar, Beijerforskare - YouTube
